
EHSRC Associate Member Snehajyoti Chatterjee, an Assistant Professor of Neuroscience and Pharmacology, led a study using spatial transcriptomic profiling to uncover the effects of polychlorinated biphenyls (PCBs) on gene expression related to spatial memory, a relevant factor in cognitive decline. The study, recently published in Molecular Psychiatry, a journal published by the Nature Publishing Group, found that mice exposed to PCBs exhibited deficits in long-term spatial memory.
To examine the molecular effects of PCB on the brain, the team used a spatial transcriptomics technique to analyze gene expression changes in five brain regions: the hippocampus, neocortex, thalamus, caudal putamen, and fiber tracts. Their analysis of spatial gene expression revealed the molecular signatures influenced by PCB in these susceptible brain regions of mice. Network analysis suggested that these changes are associated with higher chlorinated PCBs present in the brain. Additionally, the team showed that PCB exposure disrupts the expression of tight junction proteins, which are crucial for maintaining the integrity of the blood-brain barrier (BBB). Thus, the study results offer mechanistic insights into how PCB exposure affects brain function and cognition.


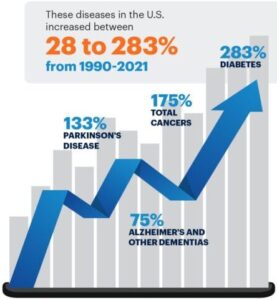 Chronic diseases including cancer, diabetes, Parkinson’s Disease, chronic respiratory disease, and childhood neurodevelopmental disorders have increased dramatically in the United States over the past few decades. Research shows that these diseases are linked to environmental factors such as air pollution, microplastics, and harmful chemical exposures.
Chronic diseases including cancer, diabetes, Parkinson’s Disease, chronic respiratory disease, and childhood neurodevelopmental disorders have increased dramatically in the United States over the past few decades. Research shows that these diseases are linked to environmental factors such as air pollution, microplastics, and harmful chemical exposures. NIEHS is at the forefront of conducting research that protects public health by revealing how environmental factors impact health and disease and supporting communities in responding to environmental disasters such as chemical spills and extreme weather events like hurricanes. NIEHS P30 environmental health research centers are at the core of this mission by advancing scientific understanding, addressing emerging public health threats, improving community health, and reducing health care costs.
NIEHS is at the forefront of conducting research that protects public health by revealing how environmental factors impact health and disease and supporting communities in responding to environmental disasters such as chemical spills and extreme weather events like hurricanes. NIEHS P30 environmental health research centers are at the core of this mission by advancing scientific understanding, addressing emerging public health threats, improving community health, and reducing health care costs. The
The 
